Smoking-induced Lung Cancer
On October 12, 1492, three ships docked on the lands of North America. Aboard the ship was Christopher Columbus and his crew. Upon arrival, he came across Native Americans. To show that his exploration didn’t mean any harm, he offered them gifts, clothes and food. In return, the tribesmen handed over dried up tobacco leaves. Confused Columbus soon realised that the leaves were a prized possession and loaded bagfuls of them overboard. Smoking was thereby introduced to Europeans, and before long, cigarette smoking became an entrenched habit worldwide.1
While loading his ship, Columbus didn’t know that tobacco smoke contains over 7000 chemicals, of which 250 are harmful and over 69 carcinogenic. He also didn’t know that tobacco would one day be responsible for 8 millions deaths/year and smoking would be the number one risk factor of lung cancer.2.3
In the 1900s, technological advancement allowed large-scale cigarette production. By the end of the 19th century, mass marketing glamorised smoking, leading to the global lung cancer epidemic in the 1940s and 1950s. Before the 1900s, lung cancer was a very rare disease. Today, it has become one of the leading causes of cancer death, and tobacco has become the main cause of 90% of male and 79% of female lung cancers.1,3
What’s in a cigarette?
The devastating link between tobacco smoke and lung cancer is due to toxic chemicals in cigarettes. As a tobacco plant grows, it absorbs chemicals, like cadmium (used in battery acid) and lead (used in batteries and house paint), from soil, both toxic and carcinogenic. During the curing process, more harmful compounds form, e.g. tobacco-specific nitrosamines.2 While manufacturing, other chemicals are added as follows:
- Nicotine – used in insecticides; it increases the release of neurotransmitters in the brain and elevates mood
- Ammonia – common household cleaner
- Acetone – used in nail polish remover
- Acetic acid – used in hair dyes
- Arsenic – used in rat poison
- Benzene – used in gasoline
- Butane – used in lighter fluid
- Carbon monoxide – released in car exhaust fumes
- Naphthalene – used in mothballs
- Methanol – used in rocket fuel
- Tar – used for paving roads
Once a cigarette is lit, more harmful chemicals are produced in the burning process that were not present initially in the curing and manufacturing processes.2
Tobacco and Lung Cancer Pathogenesis
These carcinogenic compounds activate/inactivate several signalling pathways in malignant cells. They allow cancer cells to proliferate and multiply by inducing epigenetic alterations, which help the development and pathogenesis of lung cancer.4
- Tobacco and genetic changes
TP53
TP53 is the most important tumour suppressor gene. In nearly 50% of lung cancers, DNA repairment and apoptosis induction are deregulated and mutated in p53-harbouring cells. Polycyclic aromatic hydrocarbons in cigarettes increase thymine and guanine replacement frequency in p53. Nicotine-derived nitrosamine ketone (NNK) in cigarette smoke increases substitution of guanine to adenine in exon 5 of p53. Tobacco smoke also downregulates p16 expression. It methylates the promoter region of p16. This allows cancer cells to proliferate and escape from apoptosis. Nicotine and NNK increase the expression of neurotransmitters adrenaline and noradrenaline and inhibit the expression of GABA in lung cancer cells.
Free radicals and reactive oxygen species
Every cigarette pack produces nearly 5 × 104 free radicals that induce oxidative stress and DNA damage, causing replication/transcription errors and genomic instability. In healthy cells, chemical-induced damages to single-stranded DNA are repaired by nucleotide excision repair and base excision repair (BER) systems. Xrcc1 protein in the BER system detects single-stranded breaks in DNA and acts as a scaffold for binding other repair enzymes. In smokers, polymorphisms in XRCC1 gene reduce this protein activity and disturb the DNA repair system.
β-gelatinase
β-gelatinase enzyme decomposes collagen, elastin, fibronectin, and non-matrix molecules, including pro-TNF-α, IL-8 and TGF-β. Considering its carcinogenicity, β-gelatinase releases pro-angiogenic factors and enhances tumour cell angiogenesis. It inhibits T cell proliferation and hinders immune system response by incising alpha interleukin-2 receptor, activating TGF-β and separating ICAM-1.4

Figure 1: Lung cancer progression and staging
- Tobacco and epigenetic changes
Epigenetics modulations, including DNA methylation, histone modifications, nucleosome changes and microRNAs (miR)-associated gene regulation, refer to heritable alterations in gene expression that are not due to changes in DNA sequence. These mechanisms regulate gene expression by altering the chromatin structure.
In healthy cells, DNA methylation occurs mainly in regions with a high frequency of CG sites and at 5′ end of the genes. Being repressive to transcription, the modification is catalysed by DNA methyltransferases. Different methylation patterns are reported in infants whose mothers smoked during pregnancy. Nicotine changes the expression of DNA methyltransferases, causing demethylation of synuclein-gamma oncogene. Smoking can also cause the formation of methylated tumour suppressor gene p16.
The human genome contains nearly 1600 miR—non-coding small RNAs regulating expression of several genes. Chemicals in cigarette smoke alter the miR expression pattern. MiRs regulate the expression of oncogenes and tumour suppressor genes and act as oncogenes themselves. Cigarette smoke enhances miR-504 expression, an important miR for dopamine receptor gene DRD1 expression, ultimately inducing tobacco addiction.4
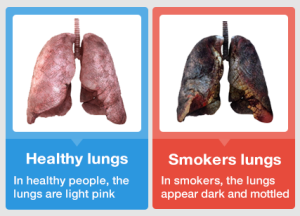
Figure 2: Healthy Lungs vs Smokers Lungs
- Tobacco and Growth Signalling pathways
Nicotine binds to nicotinic acetylcholine receptors (nAchR), epidermal growth factor receptor (EGFR) and β-adrenergic receptor (AR-β). Owing to its ability to pass through the cell membrane, in non-neuronal settings, nAchR regulates growth, differentiation and migration of cancer cells. Several signal transduction pathways, such as MAPK, AKT and PKC, become activated, which further inhibit apoptosis, stimulate tumour cell proliferation and induce angiogenesis. However, the activation and secretion of neurotransmitters through nAchR is mediated by smoking. Nicotine binds to EGFR and AR-β and acts as a growth factor. EGFR is a tyrosine kinase receptor and crucial in cell growth, development and tumorigenesis. NNK contributes to cancer cell proliferation by synthesising thromboxane A2 (TXA2) and activating the TXA2 receptor. TXA2 activates the transcription factor cAMP response element-binding protein, enhances Bcl-2 expression and increases cell proliferation.4
- Impact of Tobacco on Cell Survival, Growth and Apoptosis
Nicotine acts as a mitogen through cyclin D1 overexpression and cell cycle transition from G1 to S phase. It elevates the proliferative potential of cells by activating PI3K/AKT signalling pathway as a fundamental axis in tumorigenesis, tumour growth and drug resistance. Nicotine and NNK activate ERK and STAT pathways and disrupt anti-growth signals to increase cell growth. Cigarette chemicals suppress NK cell activity and proliferation. Defects in the apoptosis lead to cell survival and unlimited tumour cell growth. NNK and its metabolites inhibit apoptosis through upregulating hemeoxygenase (HO-1) and activating NF-κB and ERK pathway in lung tissue.4
- Impact of Tobacco on Angiogenesis and Cancer Metastasis
Angiogenesis or blood vessel formation from endothelial cells is important for nutrition and oxygen delivery to tumour cells. In one mechanism, nicotine increases the expression and secretion of nitric oxide, a vasoconstrictor and angiogenesis mediator, as well as of endothelial growth factors.
Tumour metastasis, the major cause of lung cancer mortality, is the spread of tumour cells from one organ to others. The progression and metastasis of cancer in smokers is faster than non-smokers. Prolonged nicotine use decreases the expression of adhesion molecules, such as E-cadherin and β-catenin, in lung cancer cells. Additionally, breaking the extracellular matrix using matrix metalloprotease enzymes is important for tumour cell metastasis and invasion. Also, cyclooxygenase-2 (COX-2) elevates both angiogenesis and aggressive potential of tumour cells by increasing the production of prostaglandins and converting the pre-cancerous agents to carcinogens. Nicotine enhances the metastasis of esophageal carcinoma in that it upregulates and increases the activity of MMP-2 and COX-2.4
Beyond lung cancer…
Smoking is associated with over 15 types of cancer, including breast, bladder, colorectal, larynx, liver, pancreas, kidney, ovary, mouth, pharynx, and nose and sinuses cancer. It induces cardiac and lung diseases, stroke, diabetes, and chronic obstructive pulmonary disease, including emphysema and chronic bronchitis. Smoking increases the risk of tuberculosis, eye ailments, and immune system-related illnesses, e.g., rheumatoid arthritis.
Lipid Profile Modifications
Smokers demonstrate high serum cholesterol, triglyceride, and low-density lipoprotein levels, but low high-density lipoprotein. Nicotine increases blood sugar levels, thus increasing the risk of diabetes. Diabetic smokers require high insulin doses to maintain blood sugar levels.5
Blood Cell Parameter Changes
Carbon monoxide in cigarette smoke leads to high Hb levels, increased capillary permeability, increased erythrocytes and hematocrit values and decreased plasma volume. The irritating effect of the tobacco smoke on the respiratory tree as well as nicotine-induced release of catecholamine and steroid hormones increase the leukocyte count. Smoking-induced oxidative stress causes increased platelet activation and aggregation, atherothrombotic cardiovascular events and endothelium injury caused by nicotine.
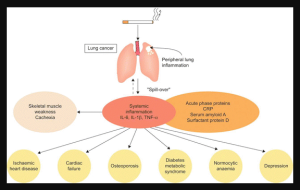
Figure 3: Smoking, lung cancer and associated comorbidities
Is there a safe level of smoking?
‘One cigarette a day is not harmful’.
‘Passive smoking won’t kill you’.
‘Cutting back is just as good’.
‘Mild cigarettes are less risky’.
‘I only smoke occasionally’.
No matter the excuses, there is no denying that ‘smoking is injurious to health’. There is no safe level of smoking. Smoking 1-5 cigarettes daily is as harmful as smoking 20+ cigarettes daily. For daily heavy smokers, the risk of lung cancer mortality is 23 times in men and 13 times in women than non-smokers.
Ways to Quit:
Tobacco urges and cigarette cravings can be strong, but if you are determined, you can stand up against these.
- Cold turkey and gradual withdrawal
- Nicotine-replacement therapy
- Avoid triggers like alcohol
- Eat fruits and vegetables
- Exercise, meditate and relax
- Delay ‘the next cigarette’
- Lean on your loved ones
Quit for Good
Cigarettes come at a great cost: your life. Irrespective of the amount and times you smoke, it’s never too late to quit.5 As soon as you stop smoking, your body starts healing itself:
- In 20 minutes, heart rate and blood pressure drop.
- In 12 hours, carbon monoxide in blood drops to normal.
- In 1-3 months, blood circulation and lung function improve.
- In 1 year, the risk of heart disease is half that of smokers.
- In 5-10 years, the risk of mouth, throat and larynx cancer is halved.
- In 10 years, the risk of lung cancer is nearly half that of smokers.
Don’t wait, quit today!
References:
- Tobacco-Free Life. History of Tobacco. https://tobaccofreelife.org/tobacco/tobacco-history/. 2016.
- American Lung Association. What’s in a cigarette? https://www.lung.org/quit-smoking/smoking-facts/whats-in-a-cigarette. July 13, 2020.
- World Health Organization. Tobacco. https://www.who.int/news-room/fact-sheets/detail/tobacco. 24 May 2022.
- Nooshinfar, E., Bashash, D., Abbasalizadeh, M., Safaroghli-Azar, A., Sadreazami, P., & Akbari, M. E. (2017). The molecular mechanisms of tobacco in cancer pathogenesis.Int J Cancer Manag. 2017;10(1):e7902. https://brieflands.com/articles/ijcm-7902.html. doi: 10.17795/ijcp-7902.
- Centers for Disease Control and Prevention. Smoking and Diabetes. https://www.cdc.gov/diabetes/library/features/smoking-and-diabetes.html. August 10, 2021.
Writer & Reviewer: Sharvari Indulkar & Dr Prachi Sinkar

