For the past 200 millennia, a war for survival has been raging between the human species and disease-causing pathogens. While our microbial adversaries were continuously mutating to gain increased virulence and resilience, our immune system developed its own mechanisms to defend against previously encountered and new infectious agents. In the 20th century, we acquired an edge in this fight spearheaded by advancements in the medicine, diagnostics and pharmaceutical fields. Rapid detection assays and effective drugs and vaccines turned the tide with a significant drop in casualties.
It was hard to imagine that a new infection would wreak a global havoc, causing loss of lives and economic devastation. The recent pandemic has once again highlighted the vulnerability of our species to disease-causing pathogens. Despite advanced healthcare systems, we struggled to effectively limit this outbreak in time, resulting in grave consequences. Medical personnel worldwide risked their lives during the pandemic to provide round-the-clock treatment and care to inflicted. It is imperative to have stringent protocols towards controlling spread and effective healthcare strategies to combat such threats. Among the most contagious diseases capable of reaching a pandemic scale was Influenza or ‘flu’, which still poses a potential threat if not addressed appropriately.
Influenza as a global epidemic
The ‘Spanish Flu’ or 1918 Influenza Pandemic was one of the deadliest disease outbreaks of the 20th century. It recorded nearly 50 crore global infections and 10 crore deaths. When it struck India in 1918, it wiped out nearly 5% of the population, i.e., 1.2 crore deaths. Three subsequent Influenza pandemics encountered in 1957, 1968 and 2009, collectively claiming around 26 lakh lives albeit with successively declining mortality rates.[1]
Origin of the Influenza virus
Although it is impossible to trace back when the first human-infecting Influenza strain evolved, historical writings from as early as 6,000 BC mention afflictions with similar symptoms. The term Influenza originated nearly in the 15th century from the Latin word Influentia translating to ‘Influence’ and was later commonly used to describe illness similar to severe cold. The microbial cause of the disease was unknown until the virus was discovered in 1892 and Influenza A was isolated in 1933.[2]
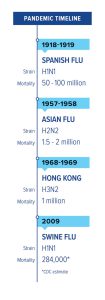
Figure 1: Timeline of pandemics in the world
Influenza and its strains
Influenza is a group of helix-shaped single-stranded RNA viruses from the orthomyxovirus family classified into A, B, C and D genera. Influenza A, B and C result in respiratory illness in humans with majority of the cases resulting from type A and B and rarely from type C. Type D is reportedly affects cattle and swine populations.[3]
| Influenza A Virus | Influenza B Virus | Influenza C Virus | Influenza D Virus | |
| Host Range | Birds, humans | Humans, seals | Humans, pigs | Cattle, pigs |
| Effects | Can result in pandemics and cause severe respiratory distress | Can result in the seasonal flu, symptoms are usually mild | Can result in local epidemics, can be severe in some cases | Bovine respiratory illness, symptoms are usually mild |
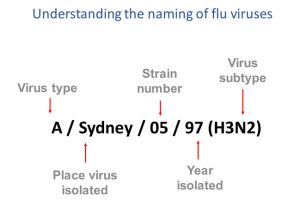
Figure 2: Naming of flu viruses
Monitoring of Influenza A or alphainfluenza virus (AIV) is considerably crucial with virulent strains capable of affecting humans pandemically. AIV is further classified into subtypes determined by surface antigens hemagglutinin and neuraminidase. Reportedly, eight H and six N subtypes infect humans. AIV was the cause of the 2009 H1N1 (swine flu) pandemic and recurring H5N1 (bird flu) outbreaks.[3]
Prevention and Treatment
Measures limiting the spread of the Influenza in 1918 were similar to those applied for COVID-19, e.g. social distancing and using masks in public. Curfews were implemented for non-essential services and personnel. Affected individuals were quarantined. The treatment involved supportive healthcare with antibiotics to prevent secondary viral infection. Although the first wave was mild, second one was remarkably more virulent. Notably, individuals who had contracted the disease in the first wave were relatively immune to the virus in the second and third waves. This provided strong evidence that the 1918 pandemic was a series of a mutated variant of the same Influenza virus. Young adults were the worst affected, and the concept of cytokine storm was then poorly understood. Older adults had acquired protective immunity from earlier influenza outbreak, exhibiting milder infections. The only treatment then effective was blood transfusions from recovered patients; however, this could not be carried out on a large scale.
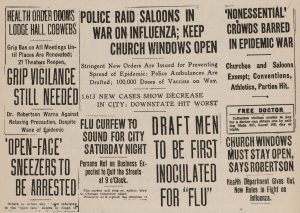
Figure 3: Newspaper articles for prevention of Influenza spread
In 2001, the frozen tissue and lung samples of victims from the 1918 pandemic were analysed to understand the cause and epidemiology of the virus. Molecular techniques used to analyze the strains revealed their ancestry to H1N1 virus. Different strains were documented with an increased virulence in the successively encountered strains due to pantropism (affecting multiple organs).[6]
Public Health Lessons
Highly contagious and often asymptomatic, Influenza spreads rapidly, especially in highly populated areas. In 1918 when the flu struck Bombay, it soon came to be known as the ‘Bombay fever’ among the local populace. By the time its lethality was ascertained, it had invaded countless households and communities. Within a few months, it reached every state with an alarming number of casualties.
An interesting article published in the Times of India on 25th June 1918 highlighted the effect on businesses and implied hope for future medical sciences to better understand and contain such diseases.
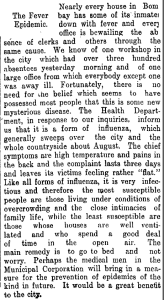
Figure 4: Newspaper article, TOI, June 25 1918
Statistical data was analysed to understand the diffusion of the virus through the population. However, this was difficult to accomplish on a large scale as various factors, including public health response, social interactions and travel patterns, are location-specific. Such analyses pinpoint vulnerabilities of specific communities to pathogenic threats, leading to better management during crisis.[4][5]
One of the factors limiting the spread of infection in the past was the lack of transport facilities. A small proportion of individuals were involved in long distance travel, which took longer by trains or ships. Today, travel is frequent with commercial airlines. As with COVID-19, it is crucial to restrict symptomatic individuals at airports. Despite such measures, asymptomatic individuals may still be overlooked, raising the requirement of rapid assays. Although rapid test kits for several diseases are developed based on the lateral flow immuno-chromatographic technique, these are not usually available for a new pathogen when it emerges. Although preventive measures limit the contagion till effective treatment or vaccines are available, it takes considerable time with clinical trials and stringent protocols for their implementation.[4][5]
For COVID-19, a global R&D initiative was undertaken by private healthcare and government sectors for vaccine development. Multiple effective vaccines were produced and disseminated by many countries among the population in a short time-frame. Vulnerable sections of society, including senior citizens and those with pre-existing conditions, were prioritized, which was followed by administering the vaccines to the entire population.[5]
Advancement in laboratory sciences and medical fields has resulted in molecular techniques that better identify and characterize the genotypic structure of pathogens, thereby accelerating vaccine development. Clearer understanding of the mechanisms involved in the transmission and manifestation of symptoms has led to effective drug therapies and supportive care. With each encountered pandemic, we have gained experience on how to mitigate and cure rapidly spreading diseases.
What should India do next?
To reduce the risk of a future endemic, we should increase the awareness about influenza as well as citizen’s responsibilities in controlling the spread of the disease. Indian healthcare system is now well-developed with a large number of competent medical personnel and advanced healthcare facilities available in nearly all parts of the country with stable access to pharmaceutical remedies. In the event of an unexpected contagion, supply of critical drugs may be hampered for a short time-frame. Controlling spread during this period could alleviate the consequences of supply concerns and buy us more time.
In India, Influenza as a threat has often been taken lightly despite our past experience. Spreading general awareness and guidelines of prevention, care and treatment could help decrease the risk and consequences in an outbreak. The initial and quick response to a new contagion is critical to completely eliminate the spread of disease. If such an event should arise, government-mandated regulations must be swiftly put together and enforced.
Healthcare facilities must have action plans ready for quarantining affected individuals. A team of medical personnel must be ready to handle such situations so as to ensure safety of themselves and patients.
Is India prepared for the next pandemic?
India has taken a strong stand with the COVID-19 pandemic. Despite our high population, effective treatment and vaccination were availed to a large proportion of masses. Research and development facilities for vaccines and drugs have successfully delivered results within a short time-frame. The robust healthcare system is capable of supportive care therapies and advanced treatment, and we now possess the knowledge and tools to fight such diseases.
Although anticipating what kind of pathogen/disease will emerge next is difficult, our citizens, government, and healthcare system must be aware and vigilant to protect themselves, their families and communities. We might face many different threats of diseases but would stand a strong chance as long as united efforts are ensured.
References:
1. Influenza Pandemic of 1918 Lessons in Tackling a Public Health Catastrophe; Economic and Political Weekly; 2021; T V Sekhar.
Reviewing the History of Pandemic Influenza: Understanding Patterns of Emergence and Transmission; McLaughlin Centre for Population Health Risk Assessment; 2016; P R. Saunders-Hastings and D Krewski.
3. Influenza Virus; Transfusion Medical Hemotherapy 2009; S. Karger
4. The evolution of pandemic influenza: evidence from India, 1918–19; BMC Infectious Diseases Volume 14 Article number: 510 (2014); Siddharth Chandra, Eva Kassens-Noor
5. Pandemic influenza – Indian experience; Lung India. 2011; J. C. Suri; M. K. Sen.
6. The Threat of Pandemic Influenza: Are We Ready?; Institute of Medicine (US) Forum on Microbial Threats 2005; Knobler SL, Mack A, Mahmoud A.
Writer & Reviewer: Kauser Jumkhawala & Dr Prachi Sinkar

